icd 9 code for hypothyroidism 2010
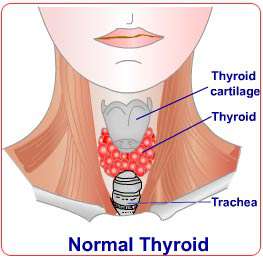
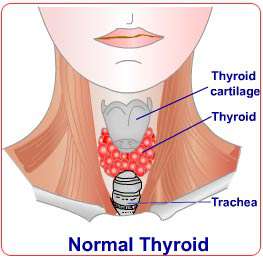
Thyroid disease impacts different factors
icd 9 code for hypothyroidism 2010 of being pregnant and postpartum wellness for the mother and also the newborn kid. There have been varied and contradicting methods in relation to thyroid disease and pregnancy. Consequently a group of endocrinologists joined together to publish a diary containing clinical recommendations for that control over an under active thyroid while pregnant and during the postpartum period. The creation of this group came into being on the two-year period as well as their results were printed in the Journal of Endocrinology and Metabolism, the July of 2007 problem. This journal signifies the methods and methods of endocrinologists all over the world.
Some of the main components of that journal are now being discussed beneath. The points keep essential implications for women who're diagnosed with thyroid illness during their pregnancy or even in the postpartum phase. Some of the info also has a bearing on women who create thyroid gland illness prior to them getting pregnant.
Hypothyroidism & Pregnancy
The health of thyroid problems inside a mother or perhaps an unborn child can cause serious health problems around the developing fetus. If a woman understands her situation as properly diagnosed hypothyroidism, she should reevaluate trying to get pregnant or steer clear of mother's hypothyroidism entirely.
If a woman should develop thyroid problems just before being pregnant and it has been correctly diagnosed by a physician or endocrinologist, her thyroid medicine will need to be modified so the thyroid stimulating hormone (TSH) level will go no greater than 2.5 prior to entering being pregnant.
A woman identified as hypothyroid throughout her pregnancy should undergo therapy instantly. The aim is to recover her thyroid gland levels normal again as soon as possible. On getting into the very first trimester, her thyroid gland-stimulating hormone (TSH) degree ought to be held below 2.5. Upon getting into the second and 3rd trimester, her thyroid-stimulating hormone (TSH) ought to be maintained below 3.. Thyroid gland function assessments have to be examined and lso are-examined inside 30 to 40 times after the initial diagnosis.
Whenever a expectant mother reaches week 4 to 6, her thyroid medicine dose will almost always need to be increased. It's possible that her dose will increase by anywhere from thirty to 50 percent.
Some women have a thyroid car-immunity as in instances where she's been formerly analyzed and discovered to be positive for thyroid gland antibodies. Woman who have an auto-defenses and who possess normal thyroid stimulating hormone (TSH) amounts in the beginning of pregnancy can still be vulnerable to becoming hypothyroid at any time in the being pregnant. Our recommendation is that she be supervised frequently throughout the being pregnant for elevated thyroid stimulating hormone (TSH).
If a woman is diagnosed with subclinical hypothyroidism that involves a thyroid gland revitalizing hormonal (TSH) degree above normal with regular totally free T4 amounts, her condition can lead to an adverse wellness end result on her and her unborn baby. Immediate treatment of mom can help to make sure a healthier being pregnant and delivery end result. Nevertheless, treatment is not proven to guarantee lengthy-term nerve improvement of the people. In spite of this, experts think that the possible benefits of treatment still over-shadow any feasible risks if the mother went without treatment. The consensus is the fact that treatment is recommended even in ladies with subclinical thyroid problems.
As soon as giving birth has happened, nearly all women who've been diagnosed with thyroid problems have to have their medication dose decreased.
Hyperthyroidism & Pregnancy

It has been found that hyperthyroidism can be
icd 9 code for hypothyroidism 2010 due to Graves' illness. Temporary hyperthyroidism may also trigger hyperemesis gravidarum, which is a situation of being pregnant that triggers severe morning illness. Diagnosing involves figuring out regardless of whether a woman includes a goiter, tests positive for thyroid antibodies or both.
If your expecting female's hyperthyroidism is triggered by Graves' illness or nodules are based in the gland, she should begin treatment for hyperthyroidism instantly. Generally, women that are pregnant receive anti--thyroid gland medicine included in treatment particularly when initially identified.
The most common antithyroid medicine given generally during the first trimester is propylthiouracil. Propylthiouracil is generally the medication of choice because methimazole consists of has a slightly greater risk of delivery flaws. Methimazole is used, but it's only recommended if propylthiouracil is not accessible or if a woman is experiencing problems with it.
You will find situations where surgical treatment could be the only suggested method for treatment rather than medicines. They're:
If there is a severe unfavorable response to anti--thyroid drugs.
If a woman demands an extremely high dose to manage her hyperthyroidism.
Uncontrolled
hyperthyroidism continues to be in spite of therapy.
Tags : How to get icd 9 code for hypothyroidism 2010,Guide icd 9 code for hypothyroidism 2010,Handbook icd 9 code for hypothyroidism 2010,Simple icd 9 code for hypothyroidism 2010,How can you icd 9 code for hypothyroidism 2010,Recommended icd 9 code for hypothyroidism 2010,To solve icd 9 code for hypothyroidism 2010,To fix icd 9 code for hypothyroidism 2010,Sale icd 9 code for hypothyroidism 2010,Bonus icd 9 code for hypothyroidism 2010